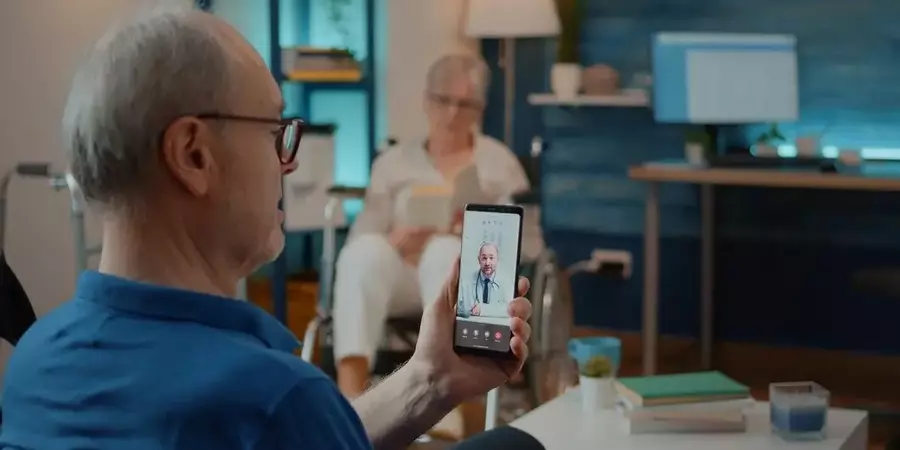
In the current landscape of healthcare, perhaps no advancement has been as transformative and timely as telemedicine. Defined as the remote delivery of healthcare services using telecommunications technology, telemedicine has revolutionized patient care, particularly in the wake of the COVID-19 pandemic. This article explores the profound impact of telemedicine on healthcare delivery, patient outcomes, and the future of medicine.
The Emergence of Telemedicine
Telemedicine, once a niche service, has rapidly gained prominence due to its ability to overcome geographical barriers and enhance access to healthcare. Initially utilized for remote consultations in rural or underserved areas, its application expanded dramatically during the COVID-19 pandemic. Lockdowns and social distancing measures necessitated a shift towards virtual care to ensure continuity of medical services while minimizing virus transmission risks.
Enhancing Access to Healthcare
One of the primary advantages of telemedicine is its capacity to improve healthcare access. For individuals in rural or remote locations, accessing specialists or even primary care physicians can be challenging. Telemedicine bridges this gap by allowing patients to consult with healthcare providers from the comfort of their homes. This convenience not only saves travel time and costs but also ensures timely access to medical expertise, thereby potentially reducing emergency room visits and hospitalizations.
Moreover, telemedicine has proven invaluable in expanding access to specialized care. Patients with chronic conditions requiring regular monitoring, such as diabetes or hypertension, can now receive timely check-ups and adjustments to their treatment plans through virtual consultations. This continuous monitoring not only improves health outcomes but also empowers patients to take a more proactive role in managing their conditions.
Improving Patient Outcomes
Beyond accessibility, telemedicine has demonstrated significant improvements in patient outcomes. Studies have indicated that remote monitoring of chronic conditions leads to better management of diseases, reduced complications, and improved patient adherence to treatment protocols. For instance, remote patient monitoring devices can track vital signs and transmit data to healthcare providers in real-time, enabling early intervention and personalized care adjustments.
In the realm of mental health, telepsychiatry has emerged as a critical tool for addressing the growing demand for mental health services. Patients suffering from anxiety, depression, or PTSD can benefit from confidential virtual sessions with therapists or psychiatrists, promoting mental wellness and reducing the stigma associated with seeking help.
Challenges and Considerations
While telemedicine offers promising benefits, it is not without challenges. Technological barriers, such as access to reliable internet connectivity and digital literacy, can hinder widespread adoption, particularly in underserved communities. Furthermore, concerns regarding data security and patient privacy must be addressed to ensure compliance with healthcare regulations and maintain patient trust.
Additionally, the effectiveness of telemedicine may vary across different medical specialties and conditions. Certain medical procedures and examinations still necessitate in-person visits for accurate diagnosis and treatment. Balancing the convenience of virtual care with the necessity of physical examinations remains a critical consideration for healthcare providers and policymakers alike.
The Future of Telemedicine
Looking ahead, telemedicine is poised to play an increasingly integral role in the future of healthcare delivery. Advances in artificial intelligence and wearable technology hold promise for further enhancing remote monitoring capabilities and predictive analytics. Integrating telemedicine into healthcare systems globally could potentially alleviate healthcare disparities and improve population health outcomes.
Moreover, the acceptance of telemedicine among healthcare professionals and patients alike suggests a paradigm shift towards a more patient-centered and accessible healthcare model. As telemedicine continues to evolve, interdisciplinary collaboration among healthcare providers, technology developers, and policymakers will be essential to navigate regulatory frameworks, ensure equitable access, and maximize the benefits of virtual care.
Improving Patient Outcomes
Telemedicine not only enhances access but also contributes to improved patient outcomes through various mechanisms. Remote monitoring, for example, allows healthcare providers to track patients’ progress continuously, enabling early detection of health issues and timely intervention. This proactive approach can prevent exacerbations of chronic conditions, reducing hospital admissions and healthcare costs.
Furthermore, telemedicine facilitates better patient engagement and education. Virtual platforms offer opportunities for healthcare providers to deliver personalized health education sessions, empowering patients to better understand their conditions and adopt healthier lifestyles. This education component is crucial for managing chronic diseases effectively and promoting preventive care practices.
Conclusion
In conclusion, telemedicine represents a transformative force in modern healthcare, offering unparalleled opportunities to enhance access, improve patient outcomes, and redefine the patient-provider relationship. While challenges persist, the rapid adoption and acceptance of telemedicine underscore its potential to revolutionize healthcare delivery beyond the constraints of traditional medical practice. As we navigate the complexities of a post-pandemic world, harnessing the full potential of telemedicine promises to create a more resilient, inclusive, and patient-centric healthcare system for the future.